Coding and Billing Chronic Lyme Disease
By: Lorna Simons, CPC
Medco Consultants, Inc
May was Lyme Disease awareness month during which celebrities such as Kelly Osbourne and Alec Baldwin described their personal stories with the disease. Though May is over, Lyme disease season continues as we get ready for the summer months.
The Centers for Disease Control (CDC) and National Institute of Allergy and Infectious Disease (NIAID) currently recommend a 2- 4 week course of oral antibiotics for treatment of Lyme disease. Many insurance carriers follow this guidance when it comes to treating the illness. This can be difficult when it comes to billing patients with continuing Lyme symptoms beyond that initial period for treatment.
The term “Chronic Lyme Disease” is a misnomer, instead the CDC and NIAID recognize Post-Treatment Lyme Disease Syndrome (PTLDS). Experts believe the symptoms of PTLDS may be caused by tissue and immune system damage caused by the Lyme disease.
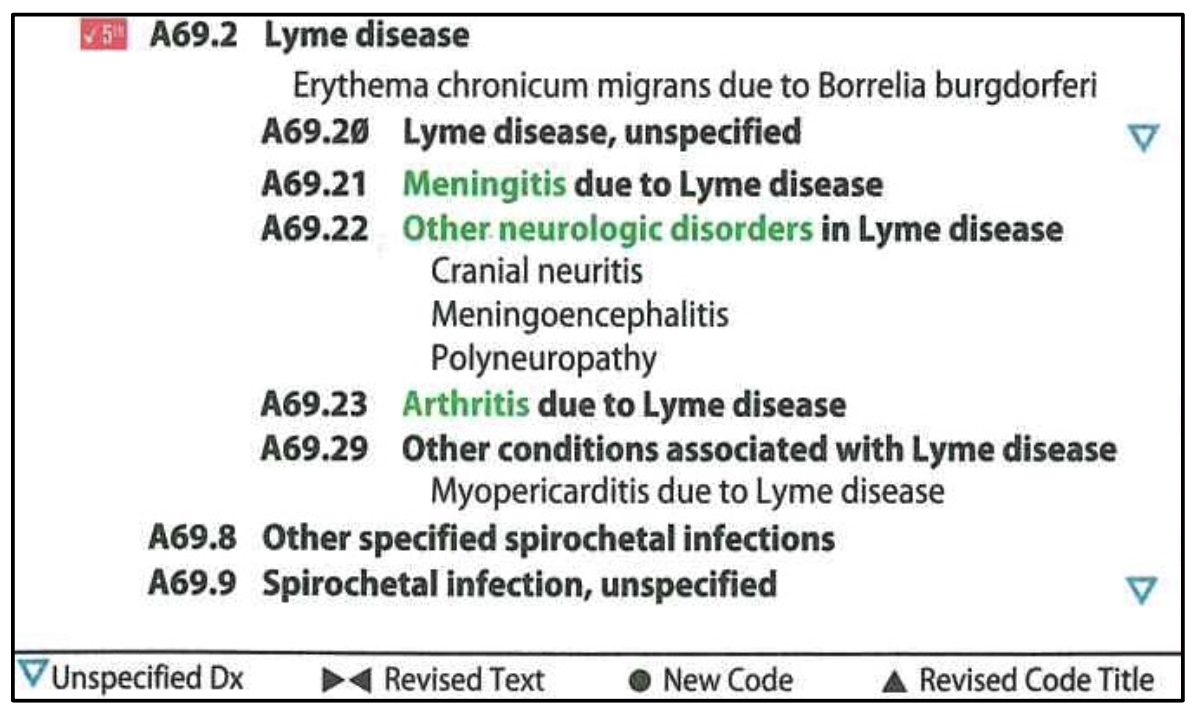
There currently is no ICD-10-CM code for PTLDS (or Chronic Lyme Disease). In the ICD-10-CM manual, Lyme disease is a subcategory with additional subdivisions. For ICD-10-CM coding of PTLDS, it would be appropriate to choose the subdivision code that most accurately describes the patient’s symptoms.
There is no current standard for treating PTLDS due to continuing disagreement in the medical community. If a patient presents with Lyme symptoms after the standard course of treatment, it is advisable to check their insurers policy for any treatment limitations. It may be necessary to provide the patient with an Advanced Beneficiary Notice (ABN) as some carriers see the treating of PTLDS with long-term antibiotics as experimental.