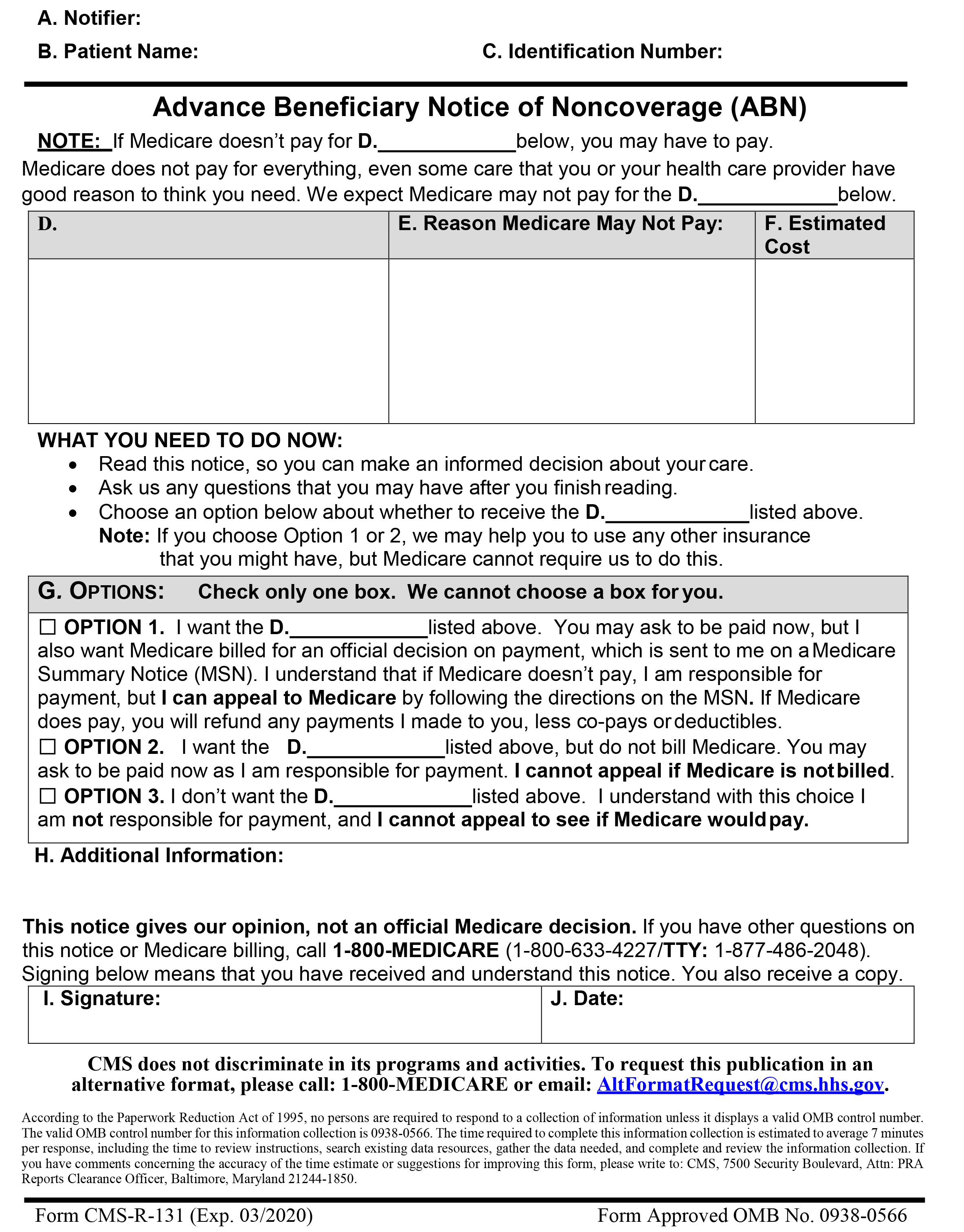
With the implementation of the electronic health record more and more providers are turning to scribes to assist with their documentation. While many providers utilize scribes, few are aware of the documentation requirements.
As we are all aware, The Centers for Medicare and Medicaid Services (CMS) utilizes Medicare Administrative Contractors (MACs) to process their claims The MACs are at the local level and they have the authority to issue documentation guidelines for their jurisdiction. Therefore, you should check with your MAC for their specific guidelines.
Having said that, there are certain documentation requirements for all MACs regarding scribe documentation.
Scribes are required to be present during the encounter documenting the word and services provided by the physician in real time.
The scribes note should include:
- The name of the scribe and a legible signature
- The name of the physician providing the service
- The date the service was provided
- The patient’s name
The physician’s note should indicate:
- Affirmation of that physician’s presence during the time the encounter was recorded
- Verification that he/she reviewed the information
- Verification of the accuracy of the information
- Any additional information needed
- Remember the physician is responsible for all documentation and is required to verify the accuracy of the scribes note.
Scribe Attestation Sample:
I, _______, M.D., hereby attest that I was present during the encounter and the medical record entry for date of service ___________accurately reflects signatures/notations that I made in my capacity as M.D. when I treated/diagnosed the above listed patient /Medicare beneficiary. I do hereby attest that this information is true, accurate and complete to the best of my knowledge.
Physician’s signature_____________________________ Date: _________
I _________________________ attest to being the scribe for Dr. ______ above named patient on ________________.
Signature of the Scribe:____________________________ Date: ________